Biography
Interests
Renata Božinović1 & Ljiljana Trtica Majnarić2,3*
1The Health Center Osijek, Croatia
2Faculty of Medicine of JJ Strossmayer University of Osijek, Osijek, Croatia
3Faculty of Dental Medicine and Health of JJ Strosmayer of Osijek, Osijek, Croatia
*Correspondence to: Dr. Ljiljana Trtica Majnarić, Faculty of Medicine, Department of Internal Medicine, Family Medicine and the History of Medicine and Faculty of Dental Medicine and Health, Department of Public Health, University of Osijek, Croatia.
Copyright © 2019 Dr. Ljiljana Trtica Majnarić, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Family physicians are among the top professions for burnout. This predisposition is in connection with their specific position in the healthcare system, at the interface with a general population. Not only a high workload but also an emotional transfer may produce a high level of chronic stress and subsequently lead to burnout. This process can be exaggerated in situations such as an economic crisis, when personal and existential factors may appear and contribute to the overall level of stress.
We conducted a survey in an eastern Croatian region, where in the last decades negative economic and demographic trends are taking place. In the group of 60 family physicians (median age 50), we found high levels of self-perceived stress and burnout, in the majority of the respondents. The factors associated with burnout included the marital status (married or divorced), children, lower physical and mental health, higher credit debts and religious affiliation. Some personality features, such as flexibility and adaptability, were identified as protective factors.
Introduction
A simple definition of the term burnout may be as “An extreme fatigue and the loss of idealism and passion for
one’s job”. The official usage of the term dated from 70ies of the 20 century, when two American psychologists,
Herbert Freudenberger, and Christina Maslach, working independently from each other, reported this condition
in their written papers as an emotional problem of providers in caregiving and service occupations, in which
the focus is on working with other people [1,2]. Although extensive research on burnout in the following
years has been conducted in the USA, Canada, and some developed European countries, this work was
based on observation and case descriptions, rather than on theoretical models. It is not surprising then, that
different definitions of burnout have been proposed and a variety of dimensions have been attributed to this
condition. Yet, most of the researches assume that what is common to all definitions, is that burnout is an
individual experience which includes negative feelings of distress, discomfort, and dysfunction, and is based
on distorted emotions, attitudes, motives, and expectations.
The dimensions of burnout on which the researchers and psychologists have achieved the best agreement include 1) emotional exhaustion, 2) depersonalization, and 3) the lack of achievement and productivity in work. The first dimension, the loss of energy and feelings, is the hallmark of burnout. The second dimension is referred to negative attitudes in relationships with others, usually expressed as irritability, cynism, and social withdrawal. This dimension is difficult to put into connection with burnout, as it is often attributed to the provider`s personality. The third dimension is referred to negative attitudes toward oneself and own personal and professional competences, expressed as depression, low self-esteem, reduced productivity and low capability for adaptation.
These responses seemed to be similar across different populations and occupational groups, which was the basis for the development of burnout measures [3]. Although the old instruments were developed from qualitative research of the founders of the discipline, and are less validated than newer measures, they are translated into many languages and are widely used among researchers [4].
Despite the ever-increasing interest of the researches and the public in burnout, it is still not included as a diagnosis in international disease classifications [1,5]. The reason is that the knowledge of etiology and psychopathology of this syndrome has not yet achieved a sufficient level of understanding [6]. It is known, e.g., that chronic occupational stress precedes burnout, but many details about the causing and protective factors and their dosing and interplay over time, are still unknown. Besides the high job demands, factors such as previous life stress events, current health status, job crafting strategies (strategies to actively change conditions at the workplace) and some personality traits, such as neuroticism and perfectionism, have been identified to play a role in the development of burnout [7]. Because employers who suffer from burnout are not only less efficient at work, but are also candidates for the development of a range of psychological and physical health problems, and reduced survival, burnout is more and more considered a public health concern.
Burnout is common in medical workers, nurses, and physicians, because of the challenging work conditions, which include the need to contentiously provide compassion to patients, the fear of medical errors, and frustrations when the effects of care provided to patients are not as expected [8,9]. The highest burnout rates have been yet recorded among primary care (family) physicians [9,10]. Some reasons for the exceptional stressfulness of this profession include high daily patient turnover, demanding patients, continuous availability to patients and decision-making in the conditions of uncertainty.
In Croatia, the situation in family medicine is dictated with the low economic situation, high rates of emigration, population aging and a high burden of chronic diseases, which is contrasted with a low doctorpatient ratio. In the eastern Croatian region, where this study was performed, the situation is even worsethan- average for Croatia. Research on burnout among medical professionals, in Croatia, is in its infancy. We aimed to assess this problem among family physicians in a larger area of the town of Osijek (currently 80. 000 inhabitants), the administrative center of the eastern Croatian region.
Methods
The survey was conducted in 2017 and included 60 family physicians, 7 men, and 53 women, the age range of 26-63 years (median 50), which is about a half of the total number of family physicians who work in the Health Center Osijek and the surrounding area. Three questionnaires were used as survey instruments. They were distributed through electronic mail, using the online Google Scholar interview computerized program. Permission to conduct the survey was obtained from the Institutional Review Boards of the Health Center Osijek and the Faculty of Medicine of JJ Strossmayer University of Osijek.
The first instrument was a free questionnaire on possible external and internal causes of chronic stress and burnout. It consisted two parts, the first one addressing demographic factors, and personal life and workplace issues, to obtain information on: age, gender, employment status (years of service, specialty in family medicine, private or state enterprise), the number of patients per day, the number of emergencies in the last week, and the number of recipes and referrals released per month (as the measures of workload), marital status, children, friendships, self-rated health, credit debts, stressful events, free time activities and hobbies, sleeping quality, smoking, alcohol and drug addiction, and religious affiliation. The second part of this questionnaire was a self-assessment of personality.
The second instrument was the Perceived Stress Scale (PSS), a 10-item questionnaire, which requires answers to the question of how often a subject has been upset in the last month because of something that happened unexpectedly [11]. The scoring is based on the 4-graded Likert scale. The score of an individual can range from 0 to 40, with higher scores indicating higher perceived stress. The score of 13 or above means a moderate level of self-perceived stress, the score of 20 or above indicates higher levels of perceived stress, and the score of 26 or above indicates a high level of self-perceived stress.
The third instrument was a burnout assessment questionnaire. It is based on answering the question: “Have you noticed changes in yourself over the past six months?”, as adapted from the Freudenberger Burnout Scale (2007) [12]. It is easy to understand for users and indicates the four burnout grades, including 1) there are things you should be worried about (score range 26-35); 2) you are a candidate for burnout (score range 36-50); 3) you are burning out (score range 51-65); and 4) you are burned out (the score above 65, to the maximum 75).
In statistical analysis, differences between categorical variables were assessed by using a Chi-square test or Fisher`s exact test. Differences between two independent numerical variables were tested by using the Mann-Whitney U test. Associations between age, burnout and perceived stress were assessed by using the Spearman`s rank correlation coefficient. The significance level was set at 0.05.
Results
The median age of the respondents was 50 years (interquartile range 33 - 55) ranging from 26 to 63 years. The median of service was 24 years (interquartile range 6 - 28) ranging from 6 months to 39 years.
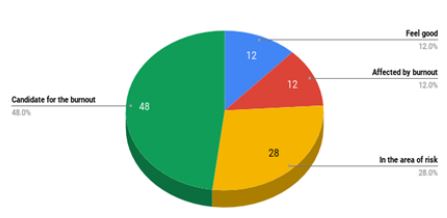
The median burnout score was 40 (interquartile range 31 - 45) ranging from 17 to 58. Most of the respondents were in the stage “candidates for burnout” 29/60 (48%) and 7/60 (12%) of respondents were affected by burnout.
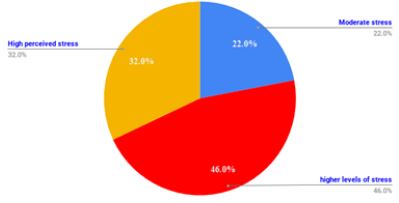
The median self-perceived stress score was 20 (interquartile range 15 - 25) ranging from 0 to 36. Almost half of the respondents were with a higher level of self-perceived stress 46% (28/60) and an additional 32% (19/60) of the respondents were with a high level of self-perceived stress.
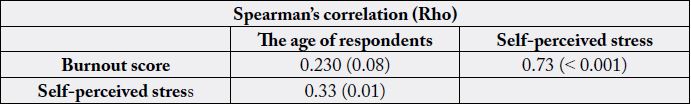
There was a strong, positive correlation between self-perceived stress and burnout score (Rho=0.73, p<0.001). The levels of self-perceived stress increased with the age of the respondents (Rho = 0.33, p=0.01) but difference in age did not affect the level of burnout.
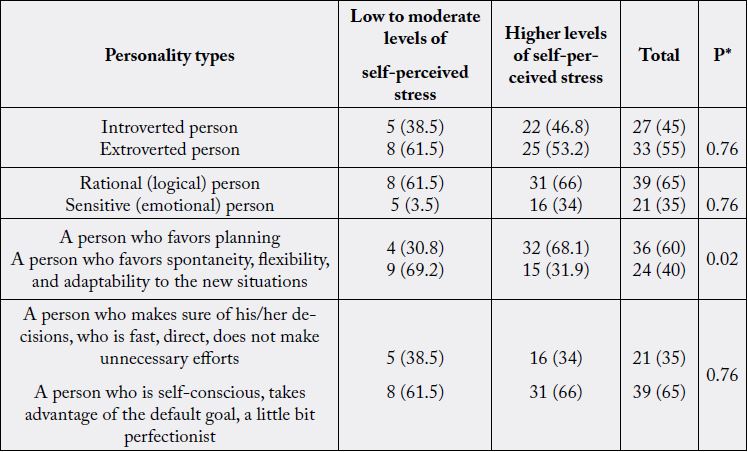
*Fisher's exact test
The levels of self-perceived stress were significantly lower in the respondents with personality types that are compatible with spontaneity, flexibility, and adaptability (p=0.02).
Of many stressful factors and determinants of burnout, assessed in this study, the results indicated that only a few of them are associated with higher levels of self-perceived stress or/and burnout. Thus, the marital status (being married or divorced), having children, lower self-rated physical and mental health, and higher credit debts, are factors associated with the status “a candidate for burnout“ or “affected with burnout“. Religious persons are more likely to be affected by higher levels of stress.
Discussion
When the respondents who in this study were candidates for burnout and those who were burned out were
taken together, this gave a high proportion of 60% of family physicians in our region, who are affected with
high levels of burnout, the number that is higher than in some other reports [10,13,14].
These unfavorable results may be in part explained by the demographic factors, such as the domination of women among family physicians (88%) and the prevalent middle age of the respondents (33 - 55 years). Women are known to more often report burnout and are more prone to emotional exhaustion and depression, than men [14]. Previous research indicated that the middle-aged and middle career medical doctors are the most sensitive to burnout [15]. This fact, as our results also indicate, may be associated with the parent`s role in this age, and not simply with the high frequency of the work-home conflicts. The problem can aggravate in the time of the economic crisis, as is the case in our region. In this situation, a parent who is a medical doctor (they are rarely unemployed and earn more money than many other common professions), may take higher responsibility for the prosperous of the family, than the partner. The worry about the existence of the family and children can exaggerate the overall level of self-perceived stress and may be a major contributing factor for the development of burnout. This scenario, in our results, is suggested with the significant association between the credit debts and burnout.
The economic crisis attacks both, the patients and the medical doctors. An increased disease burden, which in such situations usually affects the population, can be translated to medical doctors in two ways, as a higher workload, and miserable atmosphere. In exceptionally sensitive persons, or in those whose coping capacities are reduced due to personal stressful factors, this situation may lead to burnout and the development of diseases. In particular family physicians, who are in direct contact with the population, are at increased risk for the negative health outcomes. This scenario is suggested with our results. The interviewed family physicians showed a high level of self-perceived stress and this perception was in the strong correlation with high levels of burnout. Those respondents who were affected with burnout, had also worse health, than those who were unaffected. The existing diseases reduce an individual`s capacities to cope with stress, but diseases are also the final consequence of chronic stress and burnout. This overall miserable atmosphere and hopelessness, due to the bad living conditions, is difficult to quantify, and thus requires further qualitative research. The bad atmosphere at work and emotional transfer may be, however, even more important factors for burnout, than organizational aspects of the working process, as based on our results, where none of the examined workplace-related factors and indicators of a high workload, have been selected as being associated with burnout [16].
Some personality traits, such as neuroticism, have been taken into connection with a higher predisposition for burnout [1,7]. As our results indicate, some personal features, such as flexibility and good capacity for adaptation, may have a protective role. It is assumed that religious affiliation is a favorable factor when copying with stress, by allowing a transcendental delay of the real situation and emotional detachment [17]. Our results argue against this stereotype, indicating a religious affiliation as an expression of a personality trait, which might include a higher-than-average level of responsibility and/or compassion for others, and/ or a lower level of flexibility, thus representing a risk factor for burnout.
Conclusion
Although prepared on a small scale, this study was conducted on the group of family physicians who are
highly representative for burnout, as they for years work in a difficult social and economic situation. Family
physicians, who are among the top professions for burnout, may be trapped into a vicious cycle of the
interplay of the bad personal and existential factors and high occupational stress. In surroundings where
there are no psychological services or supportive peer-groups, to help them in copying with stress, as is in
our region, this vicious cycle may result in high levels of burnout, in a majority of actively engaged family
physicians. The negative consequences of this process on the patient quality of care and the doctors` own
wellbeing and health, could be catastrophic.
Disclosure and Conflict of Interests
None
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!